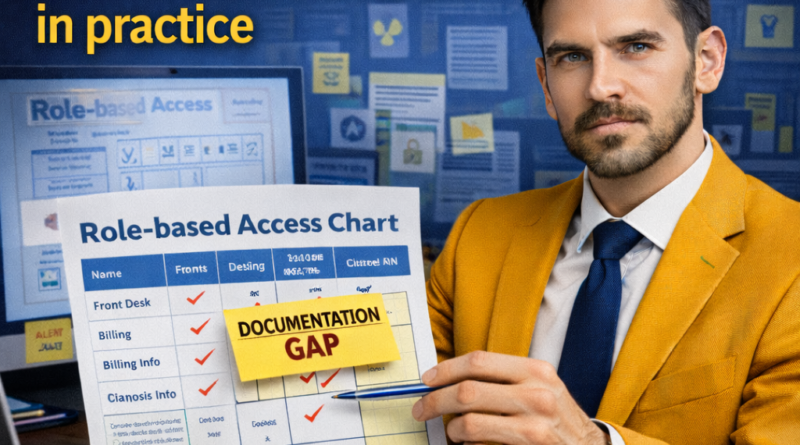
HIPAA Minimum Necessary documentation gaps in practice
The HIPAA Minimum Necessary standard often breaks down in daily operations because teams move fast, roles overlap, and access habits become “default.” When that happens, organizations struggle to explain why someone needed a specific data element, especially when disclosures involve vendors, analytics, or internal reporting.
Role-based access charts and clearly documented exceptions turn Minimum Necessary into an auditable practice. They help align workflows with privacy controls, reduce over-sharing, and create a consistent rationale when policies are challenged during reviews, complaints, or incident response.
- Over-broad access patterns can create audit exposure and remediation work
- Unclear role definitions cause inconsistent disclosures across teams
- Missing exception logic makes approvals look arbitrary
- Poor logging weakens defenses when questions arise
Quick guide to HIPAA Minimum Necessary
- What it is: a requirement to limit PHI uses, access, and disclosures to what is needed for the purpose.
- When issues arise: daily access, staff requests, vendor workflows, reporting, and non-routine disclosures.
- Main legal area: HIPAA Privacy Rule compliance and organizational controls.
- Consequences of ignoring it: excessive disclosure, weak documentation, and preventable incident response burden.
- Basic path to address it: define roles, map data elements, document exceptions, train staff, and monitor access.
Understanding HIPAA Minimum Necessary in practice
Minimum Necessary is not a promise to “never share” PHI. It is a discipline: define the purpose, identify the smallest set of information needed, and limit who can access it and how it can be used or disclosed.
In real programs, the standard is enforced through role-based access control, documented workflows, and reviewable decision points. These elements should be consistent across departments so that “needed” means the same thing in practice.
- Purpose definition: a clear reason tied to operations, care, payment, or another permitted function.
- Data element selection: the smallest set of identifiers and clinical details required.
- Role boundaries: who can access which data elements and under what conditions.
- Non-routine review: a process for requests that do not fit standard roles or workflows.
- Documentation: evidence of how the decision was made and who approved it.
- Role charts should map job functions to PHI categories and data elements
- Exceptions should be narrow, time-bound, and tied to a documented purpose
- Approvals should be consistent across departments, not dependent on personalities
- Logs should capture requester, purpose, scope, approver, and retention location
- Periodic review should retire access that no longer matches active responsibilities
Legal and practical aspects of Minimum Necessary
The practical core is simple: access and disclosure decisions should be repeatable and defensible. That usually requires written role definitions, standard access profiles, and a method to handle special requests without breaking policy.
Operationally, organizations benefit from separating routine, role-based access from non-routine disclosures. Routine paths rely on approved role charts. Non-routine paths rely on review criteria and a documented justification for scope.
- Role-based access policies: standard permissions by job category and function.
- Non-routine request review: a documented evaluation for requests outside the role chart.
- Documentation and retention: consistent storage of approvals, logs, and related communications.
- Training and reinforcement: short guidance that matches how staff actually work.
- Monitoring: periodic checks for over-broad access and unusual disclosure patterns.
Important differences and possible paths in Minimum Necessary
A common source of confusion is the difference between routine access (pre-approved by role) and one-off access (approved by exception). Treating everything as “special” creates delay and inconsistency, while treating everything as “routine” creates overexposure.
- Routine workflows: role chart governs access and standard disclosures.
- Non-routine requests: require individualized review and a scope decision.
- Vendor-enabled disclosures: need both contract controls and internal role discipline.
- Emergency scenarios: may allow expanded disclosures, but documentation still matters.
Common paths include internal alignment and documentation updates, negotiated workflow changes with vendors, and formal escalation for disputed requests. Each path should document purpose, scope, and approvals in the same standardized way.
Practical application of Minimum Necessary in real cases
Minimum Necessary issues often appear during vendor onboarding, analytics implementations, or when teams share spreadsheets, exports, or full records “just to be safe.” They also show up when staff rotate roles and keep access they no longer need.
Groups most commonly affected include operations, billing, customer support, IT, compliance, and product teams working with health-adjacent data. The friction typically comes from unclear role definitions and a lack of default data-minimized templates.
Relevant evidence and documentation usually includes access provisioning records, role definitions, request tickets, approvals, vendor statements of work, training records, and disclosure logs. Communication threads often show why scope expanded beyond the original purpose.
Further reading:
- Inventory roles and workflows that touch PHI, including vendor-supported processes.
- Build a role chart mapping job functions to PHI categories and minimum data elements.
- Define exceptions with narrow scope, time limits, and an approval standard.
- Implement logging for non-routine access and disclosures, with a consistent template.
- Review and adjust access at set intervals and after role changes or tool launches.
Technical details and relevant updates
Role charts work best when they reflect real system permissions. Align the chart with identity and access management groups, application roles, and reporting exports. The goal is to reduce “manual exceptions” by improving baseline access profiles.
Exceptions should connect to controls such as time-bound access, approval workflows, and data segmentation. If a system cannot restrict fields, the organization may need compensating measures, such as restricted exports, masking, or a separate reporting environment.
When data is shared with vendors or internal teams for analytics, a strong Minimum Necessary posture often depends on standard data sets, clear retention rules, and a defined method to refresh or delete extracts without creating unmanaged duplicates.
- Access grouping: map roles to IAM groups and application permission sets.
- Export discipline: controlled templates for reports and extracts with minimized fields.
- Retention rules: clear deletion and refresh cycles for datasets and logs.
- Periodic reviews: scheduled checks for role drift and exception renewals.
Practical examples of Minimum Necessary
Example 1 (more detailed): A revenue cycle team asks IT for access to clinical notes to resolve billing denials. The role chart allows access to billing codes, dates of service, and limited clinical summaries, but not full narrative notes. The request is routed as non-routine, and the scope is narrowed to a templated “denial support extract” that excludes psychotherapy notes and unrelated conditions. Documentation includes the purpose, requested scope, approved minimized scope, approver identity, and a retention plan for the extract. The outcome is faster resolution with less data exposure and a repeatable workflow.
Example 2 (shorter): A customer support team needs to confirm appointment status for users. The role chart grants view-only access to scheduling metadata and contact information, while exceptions require approval for any diagnostic detail. A ticketing template captures purpose and scope when an exception is requested, and access automatically expires after a set period.
Common mistakes in Minimum Necessary
- Granting full-record access because the role chart is missing or outdated
- Approving exceptions without a documented purpose and narrowed data elements
- Using ad hoc exports and spreadsheets without retention and deletion rules
- Failing to remove access after role changes, transfers, or project completion
- Relying on vendor tools without aligning internal roles and permissions
- Logging approvals inconsistently, making decisions hard to reconstruct later
FAQ about Minimum Necessary
What does “Minimum Necessary” require in daily operations?
It requires limiting PHI access and disclosures to the smallest amount needed for the stated purpose. In practice, that means role-based access profiles, standardized workflows, and a review process for requests outside routine roles. Documentation should show why a specific scope was appropriate.
Which teams most often need role charts and exception rules?
Teams that regularly handle PHI outside direct clinical care are commonly affected, including operations, billing, support, analytics, IT, and product. Their tasks often involve reporting, troubleshooting, or vendor processes where scope can easily expand. Clear role charts reduce inconsistent decisions.
What documentation is useful when a disclosure is questioned?
Useful records include the role chart entry for the requester’s function, the request ticket or email stating purpose, the approved scope of data elements, the approver identity, and a disclosure log entry if applicable. Retention and deletion notes for exports also support defensibility.
Legal basis and case law
The Minimum Necessary standard is grounded in the HIPAA Privacy Rule framework that limits uses and disclosures of PHI and supports administrative safeguards. In practical terms, it pushes organizations to avoid sharing “everything” when a narrower set of information would accomplish the same purpose.
Organizations commonly implement this through policies that define workforce access by role, procedures for non-routine disclosures, and documentation practices that allow reconstruction of why a scope decision was made. These controls also support incident response by showing deliberate minimization.
In enforcement and dispute contexts, decision quality is often assessed by whether an organization can explain purpose, scope, and controls in a consistent way. Patterns of over-broad access, missing documentation, or unmanaged exports tend to undermine defensibility.
Final considerations
Role charts and clearly defined exceptions turn HIPAA Minimum Necessary into a repeatable operational control. They reduce over-sharing, help teams move faster with approved workflows, and provide a consistent rationale when questions arise.
Strong programs focus on purpose clarity, minimized data elements, standardized approvals for non-routine requests, and periodic review to reduce access drift. Logging and retention discipline help close the loop and prevent “silent expansion” through exports and duplications.
- Organize documentation with role charts, exception templates, and consistent retention rules
- Watch timing by setting access expirations and scheduling periodic reviews
- Use qualified guidance for complex workflows, vendor structures, and non-routine disclosures
This content is for informational purposes only and does not replace individualized analysis of the specific case by an attorney or qualified professional.
Do you have any questions about this topic?
Join our legal community. Post your question and get guidance from other members.
⚖️ ACCESS GLOBAL FORUM